Addressing the structural drivers of HIV was the overarching goal of STRIVE research consortium. Over eight years, STRIVE partners investigated how structural factors create vulnerability to HIV, and what programmes work to tackle them.
What are structural drivers?
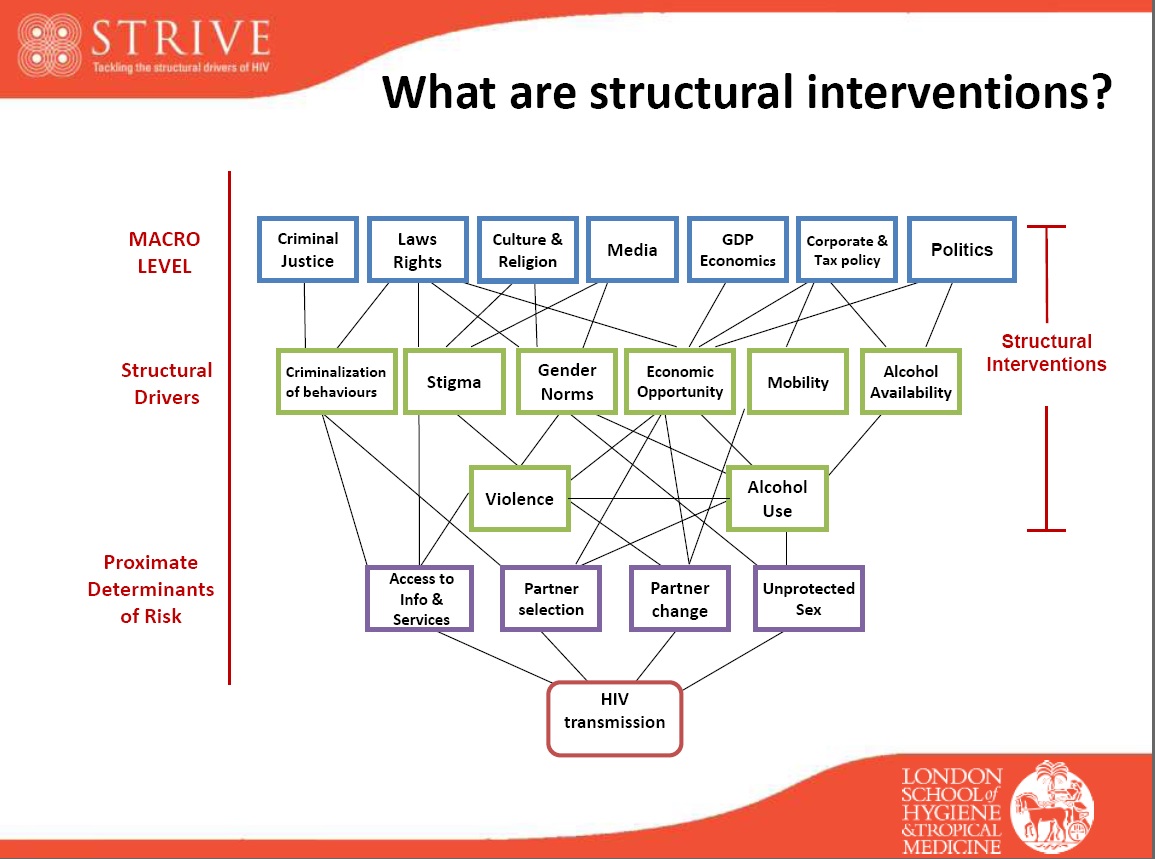
The term ‘structural drivers’ is used in HIV to describe a range of factors, acting at macro and community levels, that fundamentally shape and influence patterns of HIV risk behaviour, and facilitate or impede an individual or group’s ability to access services and/or adhere to treatment.
The conceptualisation of structural drivers considers the interplay between macro-level factors – such as laws, policies, economic conditions and cultural norms – that shape and influence patterns of behaviour and individual capacities
These macro-level factors are in turn influenced by a range of community-level factors – such as harmful gender and social norms, stigma and discrimination, violence against women and girls, and alcohol availability and promotion. Each of these may act as mediators to influence the more proximal determinants of HIV risk – such as patterns of sexual behaviour, likelihood of having a concurrent sexually transmitted infection or ability to access health services. These ultimately all influence the risk of HIV transmission.
Structural interventions aim to alter the social, economic and political contexts that influence the drivers or mediators of HIV. By targeting factors that increase people’s susceptibility to HIV at a structural level, such interventions have the potential to shift population level distributions of HIV risk behaviour and enable people at risk to benefit from the availability of prevention and treatment opportunities, and so have the potential to achieve substantial impacts.
What have we found?
- Patterns of HIV vulnerability are often complex and interconnected, and arise from combinations of structural drivers and down-stream factors
The pathways between them provide opportunities and challenges: opportunities from the potentially sustained impact of structural change, and challenges in prioritising and funding services and interventions. Indeed, evidence shows that interventions that seek to tackle these underlying vulnerabilities can achieve impact over programmatic timeframes, changing patterns of vulnerability, increasing access to and demand for biomedical interventions, and improving adherence. - Structural factors shape the current and future trajectory of HIV
Although we have had many successes in reducing the spread of AIDS, and AID-related illness and death, we will not end AIDS without paying attention to key drivers that shape risk behaviours and undermine prevention and response activities. Evidence shows that biomedical interventions such as TasP or PrEP are not sufficient without behavioural and structural support for consistent ART use. On the other hand, tackling a structural factor, such as gender inequality, must be integrated with other preventive activities if it is to achieve HIV impact. Often, the optimal HIV response requires a combination of structural, behavioural and biomedical interventions. - Structural interventions can deliver multiple benefits
STRIVE’s research shows the central importance of including responses to the structural drivers of HIV at the heart of the HIV response. For example, keeping girls in school not only reduces HIV risk, but also delays marriage and pregnancy, and improves mental health. Reducing heavy alcohol use not only reduces HIV risk but also a range of other health and economic harms. - Cross-sectoral co-financing can support interventions that yield multiple benefits across sectors
The Sustainable Development Goals provide an important framework for interventions on the structural drivers of HIV. Social and structural drivers offer investment opportunities to realise co-benefits, multiply impacts and deliver impact at scale.
Key resources
- Technical brief: Addressing the structural drivers of HIV: A STRIVE synthesis
- Learning lab: Addressing the structural drivers of HIV
- Video: Interview with STRIVE CEO Dr Lori Heise on the upstream factors that shape HIV risk
- Infographic: Tackling the structural drivers of HIV
- Summary report: The STRIVE session at AIDS2018
- Video: Presentations from the STRIVE pre-conference session at AIDS 2018



