STRIVE has developed two meta-narratives to draw together the evidence and distil the key messages for different audiences. Biomedical Interventions and the Sustainable Development Goals.
The Biomedical Interventions narrative is aimed at an HIV audience and focuses on how structural drivers impact on HIV prevention and treatment strategies.
What’s the issue?
HIV programming has tended to be vertically driven and disease specific. Since 2005, HIV prevention spending has been further concentrated on biomedical strategies such as pre-exposure prophylaxis and medical male circumcision. These strategies have contributed to an impressive 48% drop in AIDS-related deaths between 2005 and 2016.
During the same time period, however, AIDS-related deaths among adolescents and young people increased by 50%.Importantly, in hyperendemic regions, such as KwaZulu-Natal in South Africa, there was no reduction in the incidence rate of HIV in young women between 2009-2019, despite the biggest anti-retroviral treatment programme in the world.
The impact at the population level of treatment as prevention, for example, has been constrained by the realities of people’s lives. In the past, interventions to overcome barriers to the uptake focused on behaviour change. Increasingly, though, the field has come to acknowledge that individual choices are shaped at the structural level. Thus, prevention strategies must address the structural factors that inhibit or enhance the uptake of direct mechanisms of HIV prevention to achieve a population-level impact.
STRIVE set out to address two key sets of questions
- How do structural factors influence the success of biomedical prevention tools?
- Can programmes address structural factors in order to optimize the impact of biomedical HIV prevention?
What have we found?
- Biomedical interventions will not achieve the ambitious targets to end AIDS without addressing structural factors that shape HIV risk and undermine uptake and effective use.
Discussions about priorities in HIV often present behaviour, biomedical and structural interventions as being distinct policy choices. But the choice should not be between each, in isolation. Often, the optimal HIV response is likely to require a combination of structural, behavioural and biomedical interventions. - Structural factors can be addressed within programmatic timeframes with evidence-based interventions
STRIVE partners conducted a systematic review of interventions to reduce HIV-related stigma and discrimination.The review showed that considerable progress has been made over the last decade to address stigma, with the number, geographical spread and complexity of interventions expanding considerably. - We must integrate strategies to address structural factors within overall prevention, and evaluate at scale
Building on in-depth work to understand the challenges that young women face in East and Southern Africa, STRIVE researchers developed a scalable health-sector intervention called EMPOWER, which aimed to address gender-based violence in the context of a combination HIV prevention programme. They tested its feasibility, acceptance and safety in Johannesburg, South Africa, and Mwanza, Tanzania. - The HIV Prevention Cascade is an important tool to conceptualise what combination of structural, behavioural and biomedical interventions are needed to prevent HIV
As part of the Biomedical Interventions work, researchers from STRIVE produced a new framework called the HIV Prevention Cascade, which maps the steps needed to achieve high coverage of efficacious prevention tools. For any priority population that would benefit from use of a particular biological prevention method, the core steps of the cascade are: motivation to use the prevention method, access to it, effective use of it.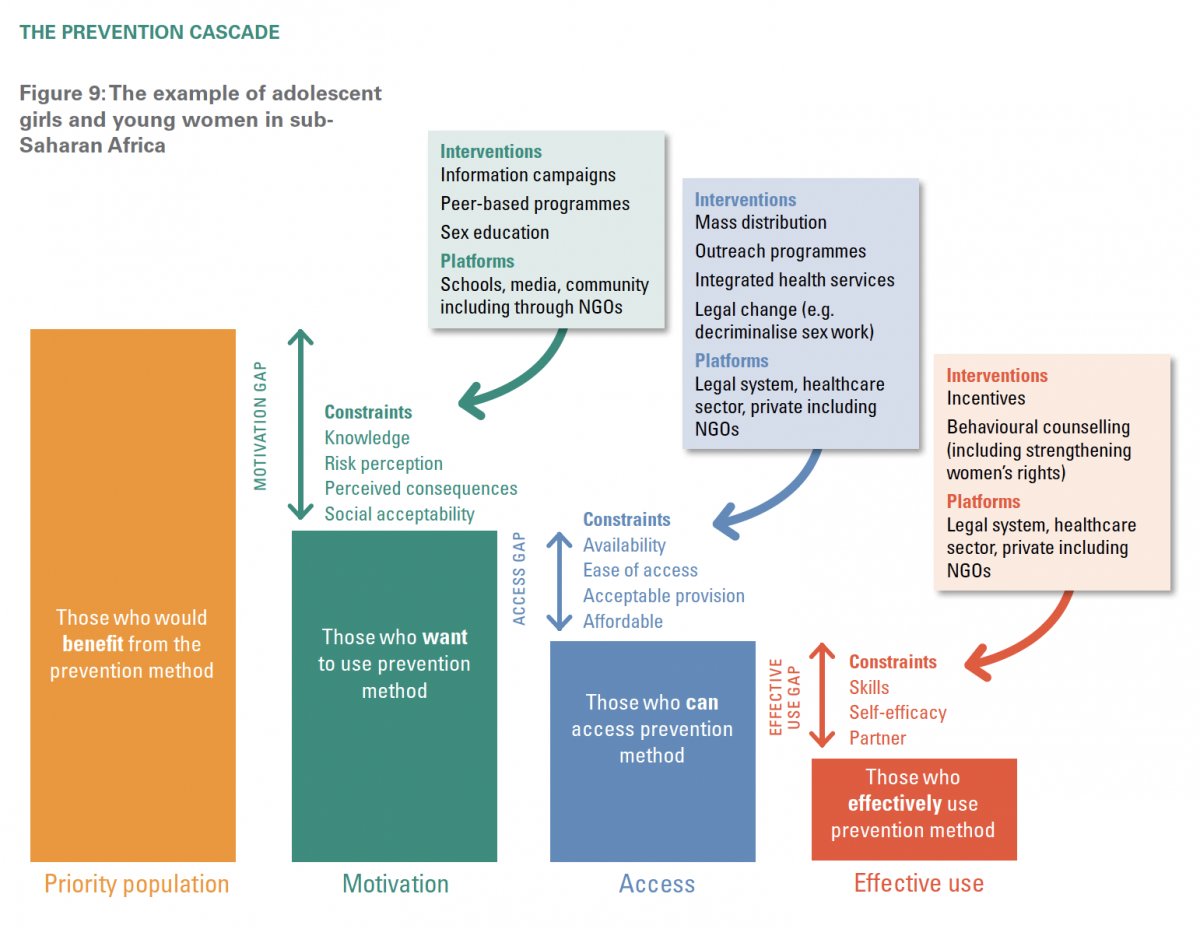
Key resources
- Technical brief: A moment of convergence: STRIVE and the Sustainable Development Goals
- Technical brief: Biomedical and structural prevention: STRIVE in the era of ‘cascades’
- Infographic: The HIV Prevention Cascade
- Learning lab: Structural factors and the HIV prevention and treatment cascades: where are we?
- Journal article: A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come?
- Evidence brief: The EMPOWER study: An evaluation of a combination HIV prevention intervention including oral PrEP for adolescent girls and young women in South Africa and Tanzania



